|
ADRENAL
NEUROBLASTOMA |
Neuroblastoma arises from the neural crest cells. 70% arise in the abdomen,
half of which arise in the adrenal gland. Neuroblastoma in situ is a benign
lesion present in 1.5% of normal neonates and is presumed to either resolve
spontaneously or develop into mature adrenal tissue (1). It has not been
described antenatally.
ETIOLOGY / PATHOGENESIS |
ULTRASOUND |
- 60-90% are in the adrenal glands (compared with only 35% of neuroblastomas in infants) (2,3).
- Usually only diagnosed in the third trimester (earlier scans on the same patients are usually normal).
- Solid.
- Cystic and anechoic (4) (50%).
- Both solid and cystic components (due to necrosis, hemorrhage and tumor involution) (5).
- Less commonly hyperechoic with calcifications.
- Usually well encapsulated and displaces the kidney inferiorly and laterally.
- Asynchronous movement between the lesion and the kidney during fetal breathing may help distinguish it from a primary renal mass.
- Usually unilateral. The right side is more frequently affected. Curtis et.al. (6) state that 90% of 31 right sided suprarenal masses were neuroblastomas. When a right sided lesion is detected after 29 weeks of gestation, the positive predictive value for neuroblastoma was 96%.
- Metastasizes to:
- Fetal liver (most common site, 25%) (7)
- Placenta (8).
- Skeleton.
- Liver.
- Neck.
- Subcutaneous tissue.
- Umbilical cord (rare).
- Fetal hydrops (several hypotheses including:
- Umbilical vein or IVC obstruction from the hepatomegaly (9).
- Hypoalbuminemia from compromised liver function.
- Mestastaic involvement of the placenta (8).
- Bone marrow infiltration resulting in anemia and cardiac failure.
- Arrhythmia due to catecholamine release resulting in cardiac failure.
- Hypersecretion of fetal aldosterone (10).
- Color doppler may demonstrate a low impedence waveform (3).
|
|
|
|
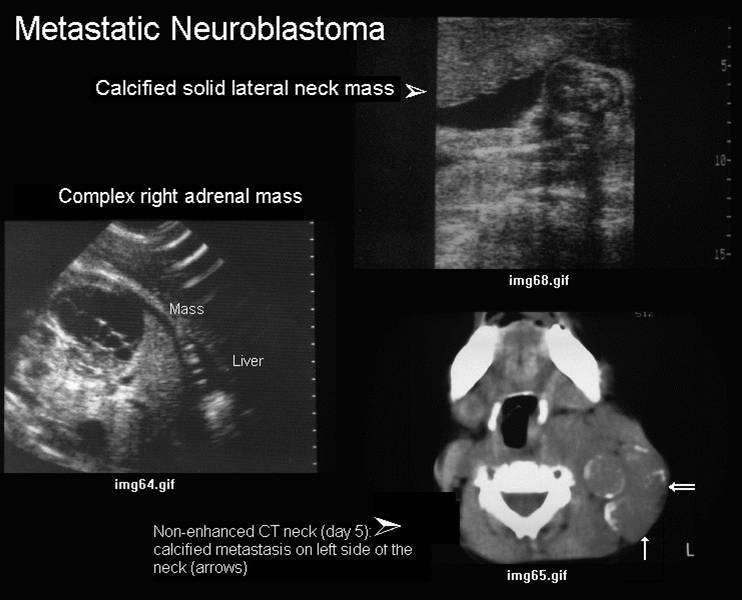
Calcified right adrenal mass |
|
|
|
|
|
Complex cystic adrenal mass with
calcified metastasis to the fetal neck |
|
|
|
|
DIFFERENTIAL DIAGNOSIS |
Link to Differential Diagnosis
REFERENCES |
- Beckwith JB, Perrin EV. In situ neuroblastoma: A contribution to the natural history of neural crest tumors. Am J Pathol 1963;43:1089.
- Acharya s, Jayabose S, Kogan S et.al. Prenatally diagnosed neuroblastoma. Cancer 1997;80:304-310.
- Goldstein I, Gomez K, Copel J. The real time and color Doppler appearance of adrenal neuroblastoma in a third trimester fetus. Obstet Gynecol 1994;83:854-856.
- Hendry GMA. Cystic neuroblastoma of the adrenal gland - a potential source of error in ultrasonic diagnosis. Pediatr Radiol 1982;12:204.
- Fenart D, Deville A, Donzeau M et.al. Neuroblastome retroperitoneal diagnostique in utero. A propos dun cas. J Radiol 1983;64:359-361.
- Curtis M, Mooney D, Vaccaro T et.al. Prenatal ultrasound characterization of the suprarenal mass: distinction between suprarenal neuroblastoma and subdiaphragmatic extralobar pulmonary sequestration. J Ultrasound Med 1997;16:75-83.
- Grosfeld J, Rescorla F, West K et.al. Neuroblastoma in the first year of life: clinical and biological factors influencing outcome. Semin Pediatr Surg 1993;2:37-46.
- Lynn A, Parry S, Morgan M et.al. Disseminated neuroblastoma involving the placenta. Arch Pathol Lab Med 1997;121:741-744.
- Van der Slikke J, Balk A. Hydramnios with hydrops fetalis and disseminated fetal neuroblastoma. Obstet Gynecol 1980;55:250-252.
- Moss T, Kaplan L. Association of hydrops fetalis with congenital neuroblastoma. Am J Obstet Gynecol 1978;132:905-906.